Arthrosis of the knee joint (gonarthrosis) is a common disease in which there is a gradual destruction (degeneration) of the cartilage tissue, followed by involvement of the surrounding structures in the degenerative process. Without the timely help of a doctor, the disease becomes the cause of severe pain and restriction of mobility, and in advanced cases leads to disability.
general information
The knee joint regularly experiences tremendous stress. Walking, running, jumping, climbing stairs and just standing up all have an impact on the condition of the cartilage. The processes of destruction and restoration are in constant equilibrium, but if, under the influence of certain reasons, this balance is disturbed, the gradual development of arthrosis begins.
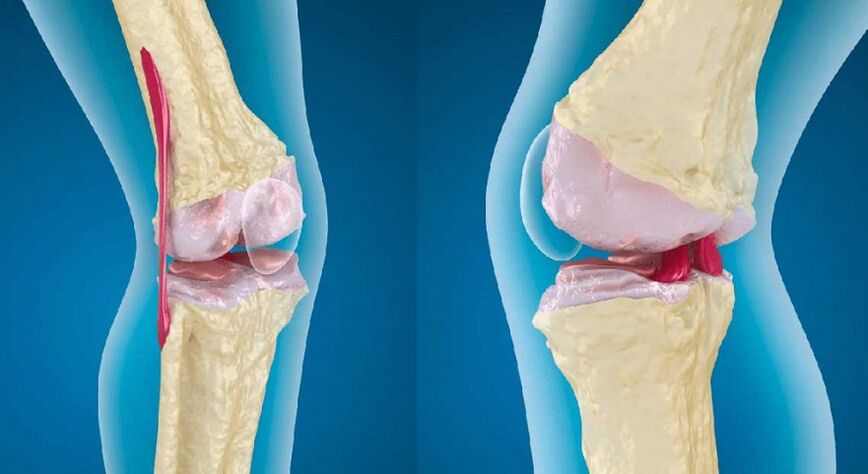
Initially, microcracks appear in the thickness of the cartilage, which contribute to a decrease in its thickness in some areas. As a result, the load on the contacting surfaces of the bones is redistributed, which accelerates the pathological process. Gradually, a whole complex of changes occurs in the knee:
- thinning of the cartilage up to complete disappearance;
- changes in the composition and reduction of the amount of synovial fluid;
- damage to bones due to friction against each other;
- the appearance of bony protrusions (osteophytes), first along the edges of the joint, and then throughout its entire area;
- compaction of the joint capsule as a result of a chronic inflammatory process, which leads to joint stiffness;
- compensatory spasm of the surrounding muscles.
Ultimately, the knee deforms significantly, and mobility is limited, which leads to a person's disability.
Depending on the localization of the process, arthrosis of the knee joint can be unilateral and affect the right or left knee, or bilateral. In this case, both legs are affected.
The reasons
Arthrosis occurs against the background of its damage due to increased stress, inflammation or congenital pathologies of the articular apparatus. The list of the most common reasons includes:
- knee injuries: dislocations, damage to ligaments and menisci, severe bruises, accompanied by hemorrhage into the joint cavity, intra-articular bone fractures;
- increased load on the joint: professional sports, lifting weights, working in a standing position, wearing the wrong shoes, overweight;
- connective tissue pathologies: systemic lupus erythematosus, rheumatoid arthritis;
- congenital and acquired weakness of ligaments and muscles, including those associated with low physical activity;
- diseases or injuries of the musculoskeletal system, accompanied by an increase in the load on the knee (flat feet, arthrosis of the hip joint);
- hormonal disorders, especially diabetes mellitus;
- metabolic disorders, accompanied by the deposition of salts (gout);
- joint inflammation (arthritis), regardless of the cause;
- knee surgery;
- heredity.
Degrees
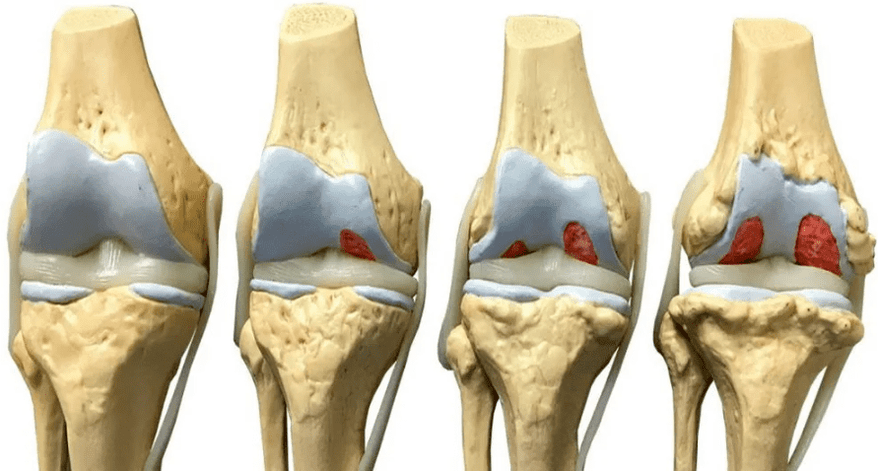
Depending on the volume of tissue damage, orthopedists distinguish 4 degrees (stages) of arthrosis of the knee joint, which determine its symptoms:
- grade 1: there are no symptoms, and minor deviations from the norm are found on the x-ray;
- grade 2: the patient notes episodic pain during physical exertion, when walking on stairs, squatting, standing for a long time; the pictures reveal a narrowing of the joint space, obvious foci of degeneration; initial manifestations of osteophytes or calcification of the lateral ligaments of the joint.
- grade 3: pain follows the patient constantly, even at rest, walking without a cane is impossible; X-ray images show a significant narrowing of the joint space, sometimes asymmetric, due to damage to the menisci, signs of joint deformation, multiple, large osteophytes, bone growths;
- degree 4: movements in the joint are practically impossible, complete destruction of cartilage and significant deformation of the articular surfaces of the bones, a large number of osteophytes are revealed on X-ray; in severe cases, the bones grow together.
Symptoms
The symptoms of arthrosis of the knee are typical for degenerative lesions. A person faces the following problems:
- pain at the initial stage manifests itself in the form of mild discomfort after climbing the stairs, and then gradually increases; with a pronounced lesion, it becomes permanent and torments the patient even at rest;
- morning stiffness: occurs already in the early stages of development, at first it lasts only a few minutes, then up to half an hour;
- crunch: occurs with the second and further degrees of damage, differs from the physiological sound in harshness and special tonality, and is also accompanied by painful sensations;
- limitation of mobility: associated with the growth of osteophytes and increased bone friction; flexion and extension of the knee is difficult and often accompanied by pain; in the last stages, the joint can be completely blocked (ankylosis);
- deformity of the knee: occurs due to a change in the shape of the contacting bones, bone growths and involvement of muscles and ligaments in the pathological process; when inflammation joins, swelling of the tissues around the joint occurs;
- lameness: as arthrosis progresses, a person limps more and more, in the later stages he is forced to use a cane or walker.
Diagnostics
Diagnosis of arthrosis of the knee joint is carried out by an orthopedist-traumatologist. To distinguish a disease from pathologies with a similar picture, as well as to determine the degree of damage, help:
- survey and collection of anamnesis: the doctor finds out the main complaints, the history of the development of the disease, learns about the injuries suffered;
- examination: reveals the degree of knee mobility, tissue deformation, especially the pain syndrome;
- laboratory diagnostics: a general blood test allows you to identify inflammation, biochemical - possible causes of problems;
- X-ray methods: X-ray and CT - the main diagnostic method that allows you to detect typical signs of arthrosis: narrowing of the joint space, osteophytes, bone deformities;
- MRI: makes it possible to visualize soft tissues, assess the condition of muscles and ligaments;
- Ultrasound: assessment of the condition of muscles, tendons, joint capsule;
- joint puncture: allows you to take an analysis of the joint fluid, as well as introduce a miniature camera to examine the cavity from the inside (arthroscopy).
If necessary, additional studies and consultations of narrow specialists are appointed.
Knee arthrosis treatment
All methods of treating arthrosis of the knee joint can be divided into three groups:
- medicinal;
- physiotherapy;
- surgical.
When a patient is diagnosed with a stage 1-2 disease, a complex of drugs and physiotherapy is used, but if the lesion has become extensive, the priority remains with surgery.
Drug treatment
The competent prescription of medications allows you to relieve pain, stop the inflammatory process, if any, and also stop or, at least, slow down the destruction of cartilaginous tissue. For this, the following groups of funds are used:
- anti-inflammatory: relieve inflammation and numb the joint;
- hormonal (corticosteroids): prescribed when anti-inflammatory drugs are ineffective;
- antispasmodics: help get rid of muscle spasms and relieve the patient's condition;
- chondroprotectors stimulate the processes of cartilage tissue regeneration;
- drugs to improve microcirculation: improve the supply of oxygen and nutrients to the joint.
Depending on the situation, tableted, injectable and local forms of drugs are used, intra-articular administration is allowed. Only a doctor is involved in the selection of drugs, their dosage and frequency of administration. When used uncontrollably, many drugs can worsen the condition of the joint, as well as cause unpleasant side effects.
Physiotherapy
Physiotherapy techniques are used to improve blood circulation in the joint area, increase mobility, and enhance the action of drugs. The doctor may prescribe:
- shock wave therapy: ultrasound of a special frequency, helps to eliminate osteophytes;
- magnetotherapy: exposure to a magnetic field that stimulates metabolism and regeneration processes;
- laser therapy: deep heating of tissues with a laser beam;
- electrotherapy (myostimulation): the effect on muscles with a weak electric current;
- electro- or phonophoresis: the introduction of drugs (chondroprotectors or analgesics) using an electric current or ultrasound;
- ozone therapy: the introduction of a mixture of gases into the articular cavity.
According to individual indications, physiotherapy exercises and massage are also prescribed.
Surgery
Surgical treatment of knee arthrosis is prescribed when other methods are ineffective. Doctors carry out several options for operations:
- endoprosthetics: complete replacement of a damaged joint with a prosthesis;
- arthrodesis: bonding bones together to eliminate mobility (allows you to reduce pain and enable a person to lean on the leg);
- osteotomy: dissection of one of the bones and positioning it at an optimal angle to reduce stress on the joint.
Arthrodesis and osteotomy are used when it is impossible to carry out endoprosthetics or if it is necessary to postpone this operation for some time.
Prophylaxis
To maintain the health of your knees, you must adhere to the following rules:
- lead an active lifestyle, engage in amateur sports, walk more and do exercises;
- avoid stress and overwork;
- minimize the risk of injury;
- keep weight within normal limits;
- eat properly and in a balanced way;
- wear high quality orthopedic shoes;
- avoid excessive stress on the knees (lifting weights, professional sports, prolonged leg work).
The same rules are relevant for those who already suffer from arthrosis, because their observance helps to slow down the development of the disease.
Diet
The condition of the cartilage depends largely on the quality of nutrition. With signs of arthrosis, it is recommended to exclude:
- carbonated drinks;
- alcohol;
- excessively fatty and spicy foods;
- canned food and semi-finished products;
- products with artificial colors, preservatives, flavors.
The diet should contain a sufficient amount of protein, fatty acids (especially omega-3), collagen (found in gelatin, agar-agar). It is necessary to build the menu so as to prevent an increase in body weight.
Consequences and complications
Arthrosis of the knee joints develops very slowly, but if untreated, this disease becomes the cause of serious and unpleasant complications:
- severe deformity of the joint and leg, in general (associated with a change in the configuration of the knee, as well as the restructuring of the muscular frame and curvature of the bones);
- shortening of the limb due to grinding of the heads of the bones;
- ankylosis: complete lack of movement in the affected knee;
- damage to other parts of the musculoskeletal system due to improper distribution of the load (heel spur, arthrosis of the hip joint, pain in the spine).
In order to prevent these problems, it is important to undergo an examination by an orthopedist in a timely manner and follow his recommendations. Self-medication and enthusiasm for folk remedies can seriously aggravate the situation.
















































