Disease: arthrosis of the joints
Which organs are affected: joints (most often the joints of the limbs)
Causes: local (related specifically to the joint), systemic (a consequence of malfunctions in the body), external (as a result of surgery or injury)
Symptoms: aching pain, crunching in the joint when moving, aches, swelling, fever, impaired mobility
Complications: destruction of the joint, hernia in the intervertebral discs, the development of arthrosis in other joints
Doctor: rheumatologist
Treatment: medication, local, physiotherapy, massage, gymnastics, diet, surgical treatment (arthroplasty, prosthetics)
Prevention: reduction of physical activity, health control
What is it?
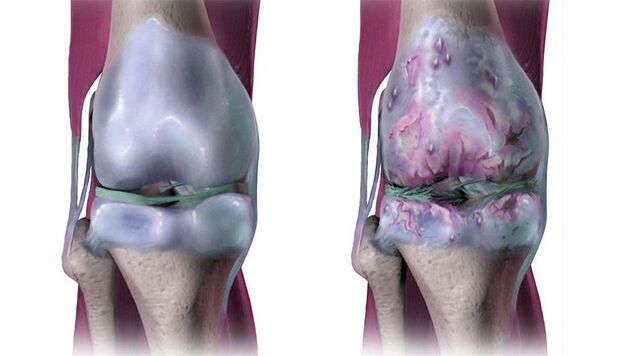
Arthrosis is a chronic degenerative disease of the joints, which is expressed in their destruction. In this case, all structures of the articulation of the joint are damaged - cartilaginous, bone, connective tissue (ligaments and the articular bag). The disease is widespread: from 6-7 to 10-15% of the population of different countries suffer from it. Thus, in the United States, 32. 5 million adults suffer from arthrosis. Most often, this percentage includes people over 45 years old, but patients are also younger.
Causes of arthrosis
There are a lot of reasons for this disease, all of them can be reduced to several groups.
Local
The problem is related to the affected joint itself. These are weak muscles, dysplasia or abnormal mobility (hypermobility) of the joint, the pathology of its development.
System or internal
When the destruction of cartilage is a consequence of other malfunctions in the body. For example, an imbalance in sex hormones can lead to arthrosis. In women, estrogen deficiency leads to osteoporosis - a decrease in bone density and its destruction. In this case, the bony surfaces of the joints also suffer. They are also affected in other metabolic disorders: diabetes mellitus, dyslipidemia (imbalance between "bad" and "good" cholesterol in the blood). The tendency to this disease can be inherited. A bacterial or viral infection can cause arthrosis. Excessive body weight with obesity can also provoke arthrosis.
External factors
Trauma or joint surgery can cause arthrosis. Arthrosis of the joints of the foot can be earned if you wear too tight and uncomfortable shoes, and the knee and hip joints begin to collapse in those who have to walk and stand a lot, lift weights (athletes, loaders).
Who is at risk?
Osteoarthritis occurs mainly in old and senile age. Most susceptible to the disease:
- People who have suffered a joint injury or lead a lifestyle that is associated with increased stress on the joints;
- Elderly people (the risk of developing arthrosis increases with age);
- Women over 50 years of age (the risk of developing arthrosis in women in old age is higher than in men);
- Overweight people (overweight can cause the development of arthrosis of the hip and knee joints);
- People with a family history of arthrosis.
On average, in different countries, arthrosis occurs in 11-13% of residents. The rate will rise as life expectancy increases and the proportion of obese people rises.
Forms and stages of the disease
The disease is classified according to several parameters. Arthrosis is called primary or idiopathic if, at first glance, it develops for no obvious reason. Most often, this type of arthrosis occurs in people over 40–45 years old. It is distinguished by the destruction of not one joint, but several at once.
Secondary arthrosis has a clear cause. As a rule, it is provoked by injuries and all kinds of malfunctions in the body due to congenital, acquired or endemic diseases, metabolic failures, hormonal disorders, neuropathy, and calcium metabolism disorders.
Among the common forms of secondary arthrosis:
- Psoriatic (as a complication of psoriasis, mainly large joints are affected);
- Gouty (a consequence of a violation of the metabolism of uric acid, under attack, first of all, small joints - the interphalangeal joints of the feet);
- Rheumatoid (heredity is of great importance, caused by autoimmune aggression against the tissues of the joint);
- Reactive (its mechanism is triggered by an infection, and arthrosis becomes a response to it);
- Post-traumatic (after injury if treatment has failed).
Depending on the latitude of the lesion, arthrosis is divided into local (up to 3 joints are affected) and generalized (more than 3 joints are affected).
There are 4 stages of pathology development:
Presumptive arthrosis
The disease almost does not cause discomfort, the mobility of the joints is preserved. Pathological changes in the cartilage are already present and amount to at least 10%, the muscular apparatus is weakened.
The initial stage of arthrosis
The pain is moderate, but constant. Joints begin to "click", muscle work is disrupted. The joint gap narrows. The X-ray shows the destruction of the cartilaginous structures (defects and cracks). The first pathological growths in the form of thorns appear on the bone - osteophytes.
Moderate arthrosis
The joint loses its mobility. The muscles around him are either shortened, or severely weakened, and poorly contract. The reduction in the joint space is moderate. Damage to the cartilage tissue spreads (cartilage detachment) to the bone.
Severe arthrosis
The joint is severely deformed due to advanced degenerative processes. The surfaces of the joint are exposed and covered with ulceration. The axis of the limb changes, the ligaments are shortened, this leads to limited joint mobility. The muscles around the joint are either shortened, or severely weakened, poorly contracted. The joint gap is significantly reduced, more than 60% of the cartilage is damaged. On the bone there are large osteophytes.
Arthrosis can result in complete destruction of the joint and lead to serious impairment of mobility.
How is arthrosis different from arthritis?
Do not confuse arthritis and arthrosis: in the first case, we are talking about an inflammatory process, and in the second - about a degenerative process, that is, the destruction of the joint due to wear under the influence of increased loads or simply with age. These phenomena almost always accompany each other, but are not identical.
Another question: what is the difference between arthrosis and osteoarthritis (osteoarthritis)? It does not exist: according to the International Classification of Diseases (ICD), these are different formulations of the same diagnosis.
Symptoms
Arthrosis is a chronic disease. It develops gradually, among the symptoms of arthrosis:
- Aching pain from barely noticeable to severe - depending on the scale of the disease. Exacerbation occurs during physical activity - walking up stairs or squatting. With the deterioration of the condition, the pain pursues even at rest. Discomfort sometimes appears without additional stress, towards the end of the day.
- Cracking in the joint when moving, aches. The first of these symptoms is initially silent - the patient feels the click rather than hears. Over time, this sound can be heard by others. Breaking, twisting the joint begins most often with hypothermia.
- Edema is swelling of the surrounding tissue. Most often appears at the advanced stages of arthrosis or with its exacerbation. The joint itself is also enlarged and deformed.
- Temperature rise. Usually local, in the area of the collapsing joint, if inflammatory phenomena join the degenerative changes.
- Mobility impairment. When the cartilage and articular surfaces of the articulating bones are severely damaged, movement in the joint becomes difficult.
Important!All these symptoms appear when the disease has already affected the periosteum. Before that, the disease often does not manifest itself in any way. Therefore, you should from time to time be examined by a specialist in order to exclude the latent course of arthrosis.
Which joints are most commonly affected?
The first to suffer with arthrosis are large joints, which bear the greatest load. Certain types of arthrosis, which are more common than others, have received their own names:
- Gonarthrosis is a lesion of the knee joint. In this case, the patient feels discomfort under the kneecap or on the inside of the knee. On palpation (probing) of the affected area, pronounced aching pain is determined. As the disease progresses, flexion and extension of the knee is limited.
- Coxarthrosis is a lesion of the hip joint. It happens as a result of congenital dysplasia or trauma. Discomfort is felt while standing, even without load. There is no swelling, there is moderate soreness when palpating. Over time, a limb (one or both) is shortened, which causes lameness or waddling gait, atrophy of the thigh and gluteal muscles.
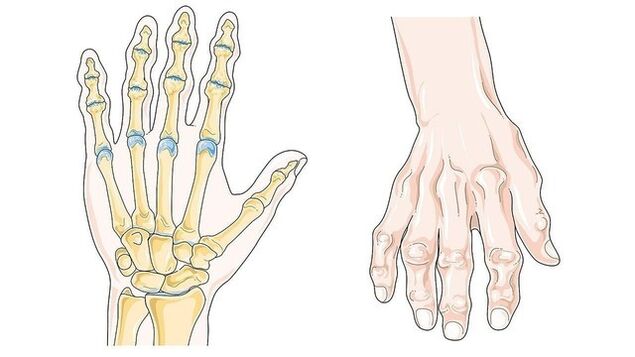
- Rhizarthrosis. The main symptom is compaction, enlargement of the joints on the hands, a significant deterioration in their mobility. Small joints of the hand are most often affected. Manifestations: bone formations on the distal phalanges of the fingers (Heberden's nodes, Fig. 3), on the intermediate phalanges (Bouchard's nodes), damage to the thumb due to trauma or senile degeneration, destruction of the wrist joint.
- Uncoarthrosis is a lesion of the cervical spine. Bony growths - osteophytic thorns narrow the spinal canal, press on the nerve roots and walls of the arteries, causing neck pain with spread to the arms, headache, blurred vision, fluctuations in blood pressure.
Also, joints of other localization may suffer - ankle, spine, elbows, shoulders, and other joints.
As a rule, the disease proceeds in waves with a change in the stages of exacerbation and remission. Therefore, it is difficult to diagnose arthrosis on your own, a specialist should do this.
Diagnostics
Examination in case of suspected arthrosis is carried out by a rheumatologist, in some cases it may be necessary to consult other specialists (endocrinologist, surgeon, orthopedist, etc. ). The diagnosis is made after analyzing the patient's complaints, examination, X-ray and laboratory tests.
They say about the probable presence of arthrosis:
- characteristic symptoms (joint pain, which increases with exertion, stiffness is felt mainly in the evening),
- advanced age of the patient.
More research is needed to rule out other conditions with similar symptoms, such as fractures and rheumatoid arthritis.
Treatment
Therapy for arthrosis, as a rule, is complex and, in addition to taking medications, includes adherence to a diet and exercise therapy.
Drug treatment
Treatment of arthrosis often involves the use of a whole range of drugs. Each group of drugs has its own goals of use (Table 1).
Table 1. Drug treatment for arthrosis
| Group of drugs | Purpose of therapy |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | Reducing pain and relieving inflammation |
| Chondroprotectors (drugs based on glucosamine and chondroitin) | Prevention of further cartilage destruction |
| Hyaluronic acid injections | Prevention of friction in the joint, relieving pain, activating the natural production of lubricant. Used after elimination of inflammation |
| Corticosteroids | Used for severe illness, if NSAIDs do not cope with inflammation and pain |
Local treatment
Topical preparations are effective in the complex treatment of exacerbation of arthrosis. Most often, they use warming and analgesic ointments and compresses based on an anti-inflammatory substance.
Physiotherapy, massage, gymnastics
Massage of the affected areas can be done during remission. It reduces discomfort, improves nutrition of the joint tissues, and restores normal joint mobility. Massage course - from 20 to 30 sessions lasting from 10 to 20 minutes.
It is important not to forget about motion therapy - performing a number of special exercises. They will not restore the joint, but they will not allow muscles to atrophy and ligaments weaken. Gymnastics is started only during remission.
Patients with arthrosis are often prescribed a course of physiotherapeutic procedures: heating, laser exposure, electrophoresis, oxygen therapy. Magnetotherapy, ultrasound therapy, shock wave therapy, and cryotherapy are often prescribed.
Important!It is useful for patients with arthrosis to be treated with mud and take mineral baths - salt, iodine-bromine and others.
Diet
A common cause of joint destruction is overweight. It is important to monitor your diet in order to normalize body weight and reduce stress on joints. But even if arthrosis is not associated with extra pounds, adjust the diet anyway. The therapeutic diet is based on the following principles:
- Balance. It is important to prevent both vitamin deficiency and hypervitaminosis.
- Energy control. It should not exceed the daily energy expenditure (overweight or obese patients reduce calories to lose weight).
- Fatty meats, concentrated broths, canned food and semi-finished products are excluded.
- The amount of salt in the diet is reduced to 5 grams per day, or it is completely abandoned.
- Fluid intake should be sufficient - at least 2 liters daily.
- The diet involves up to 2 fasting days a week. During this period, the amount and variety of food is limited. For example, kefir days - 1. 5-2 liters in several doses per day and nothing more.
Important!Foods with mucopolysaccharides - natural protectors of articular cartilage (chondroprotectors) - are very useful as part of the diet. These are cartilage, red fish, gelatin, chicken meat. You can cook jelly, make fish jellied, fruit jelly.
Surgery
With advanced stages of the disease, drug therapy is ineffective. In this case, surgical intervention may be recommended:
- Arthroplasty. The cartilage is replaced with a special pad. This significantly reduces pain and improves mobility.
- Prosthetics. If the scale of the disaster is too great, only replacing the destroyed joint with a special graft will help. It is made from a medical alloy that the body does not reject. The lifespan of such a prosthesis is about 10 years.
Forecast
Arthrosis is a chronic pathology. It is completely impossible to recover from it. The disease develops rapidly without treatment, impairing the patient's mobility and leading to disability. However, if the patient seeks a doctor on time and follows all the recommendations, the worst-case scenario is often avoided.
Prophylaxis
Any disease is easier to prevent than to cure. Arthrosis is no exception. To prevent it, it is enough to observe the following rules:
- Eat a balanced diet
- Organize moderate physical activity every day,
- Prevent hypo- and hypervitaminosis,
- Do not run chronic diseases
- Keep track of your weight
- Do not carry weights.
Conclusion
Arthrosis is a chronic degeneration (destruction) of the joints. The disease can develop due to extra pounds, metabolic disorders, permanent injury, with excessive physical exertion in athletes, dancers, etc. Large (knee, hip, shoulder, elbow) and small joints, including the spinal column (spondyloarthrosis), are affected. Without treatment, the pathological process in the joints is gaining momentum, which can end in a wheelchair. Crunching, pain, a feeling of "jamming" in the joint is a reason to consult a rheumatologist.
















































