Arthrosis or osteoarthritis of the hip joint (coxarthrosis) is a gradually developing, chronic destruction of articular cartilage and joint bones.
With pathology, the composition of the synovial fluid (fluid in the joint cavity) in the joint capsule of the pelvic region changes. The cartilage tissue loses its elasticity, density, and becomes covered with cracks. The pressure on the bone increases, this contributes to the appearance of marginal growths (thorns or osteophytes along the edge of the joint), the formation of cysts and erosions. There is a degeneration of tissues, loss of their functions and destruction.
Pathology appears due to:
- constant stress (for example, due to sports training or overweight);
- aging (age after 60 years);
- decrease in the resistance of cartilage tissue due to various diseases: for example, reactive arthritis, rheumatoid arthritis; in the structure of the cartilage, the content of water and collagen decreases, it is rapidly destroyed even under normal loads (walking, running).
At the beginning of the disease, a person feels pain when walking, after exertion. A little later, lameness joins the symptoms towards the end of the day.
Over time (on average after 3-5 years), pathology can cause limitation of active movements (flexion, rotation, extension of the hip), partial or complete disability (this happens in 98% of cases).
Coxarthrosis (hip osteoarthritis) is incurable. It progresses throughout life.
If at the beginning of the development of the disease (stage 1–2) the changes can be stopped, then at later stages (stage 3–4) the problem is solved surgically.
If there is a suspicion of a disease, they turn to a rheumatologist, orthopedist.
The mechanism of development of the disease
The hip joint consists of the head of the femur and the acetabulum, covered with smooth cartilage. They provide a smooth glide of the head while driving.
Under the influence of a number of factors, the tissues of the joint age faster:
- Pathology begins with a change in the composition of the articular fluid.
- There is a metabolic disorder, "starvation" and death of cartilage cells (chondrocytes).
- Over time, the articular surface loosens, loses its elasticity and strength, and cracks.
- The shock-absorbing functions of the cartilage deteriorate, the pressure on the bones increases.
- Broken pieces of cartilage provoke the development of inflammation and reactive synovitis (inflammation of the joint membrane after an infectious disease - influenza, enterovirus infection, measles, etc. ).
- Bone tissue becomes denser, foci of ischemia (disturbed blood supply), cysts, erosion appear in it.
- To compensate (reduce) the pressure on the bone, the cartilage grows and ossifies along the edges, forming spines (osteophytes).
As a result, the articular surfaces of the bones are destroyed, the joint is deformed, and movements in it are limited. The surrounding muscles noticeably decrease, lose strength (atrophy).
At subsequent stages of the disease, the gait is deformed (reminiscent of a "duck"). The patient waddles from foot to foot, begins to limp severely, can hardly move, and eventually becomes disabled (cannot take care of himself and walk without assistance).
How to treat arthrosis of the hip joint? Medicines are effective at the first stage, at the next stage, surgical intervention is the way out.
Causes of arthrosis of the hip joint
The reasons for the development of pathology:
- excessive load on the joint (sports training, profession features, overweight);
- a decrease in the strength of the articular cartilage against the background of chronic pathology (for example, with rheumatoid or reactive arthritis).
The development of the disease can provoke a number of conditions:
| Processes provoking the development of arthrosis | Pathologies that reduce the strength of the joint |
|---|---|
Injuries, injuries (fractures, cracks, ligament ruptures) |
Arthritis (joint inflammation) |
Operations: for example, removal of the meniscus, plastic (restoration of integrity) of the ligaments |
Metabolic problems (gout, hypoestrogenism (decreased levels of the hormone estrogen in the blood) during menopause in women) |
Impaired leg stability (flat feet; dysplasia - abnormal tissue development as a result of congenital disorders) |
Tumors (sarcoma, cysts) |
Spine problems (scoliosis) |
Systemic connective tissue diseases (rheumatoid arthritis, systemic lupus erythematosus) |
Weakening of muscles, ligaments around the joint |
Hemarthrosis (capsule hemorrhage) |
Hypothermia (hypothermia) |
Osteochondropathy (aseptic, that is, proceeding without the participation of microorganisms, necrosis (tissue necrosis) of the bone) |
Physical inactivity (insufficiently active lifestyle) |
Chondromatosis (congenital malformation of bone tissue associated with impaired cartilage formation) |
Disruption of blood supply to tissues (muscles, ligaments) around the joint |
|
Osteochondrosis |
Risk factors:
- gender (in men, the disease develops less often);
- heredity (the probability of illness of relatives increases 2-3 times).
Three degrees and 4 stages of pathology
The disease develops in several stages. Each degree of pathology is characterized by certain changes:
Three degrees of illness
| The degree of arthrosis | Characteristic changes |
|---|---|
one |
Pain in the thigh area after exercise, sometimes radiating to the knee - usually disappears after sleep or rest |
2 |
|
3 |
|
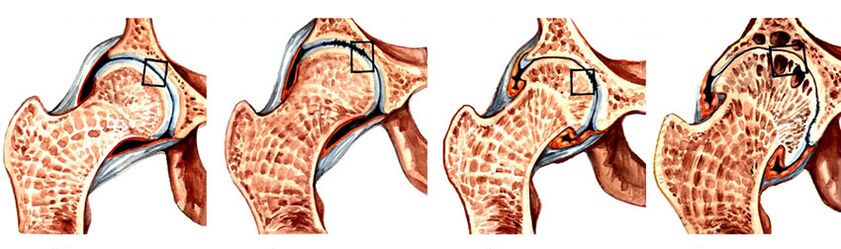
Four stages
In coxarthrosis, there are 4 stages of changes that can be seen on an x-ray.
| Stages | Signs of coxarthrosis on X-ray examination |
|---|---|
one |
|
2 |
|
3 |
|
four |
Complete fusion of the joint space (concomitant symptoms correspond to grade 3 of the disease) |
Typical symptoms at different stages of the disease
In the early stages, a person experiences pain after exercise. Gradually, the signs of arthrosis increase, the pain intensifies, they are felt constantly, after rest they do not disappear.
At stages 2-3, the gait changes to a waddling gait, reminiscent of a "duck" gait. A person begins to take care of a limb, step more carefully and not overload - as a result, the muscles in it atrophy, and it becomes shorter than the other, and lameness appears.
As the disease progresses, it becomes more difficult for the patient to bend over and move the hip. In the last stages, deformation of the joint occurs, which becomes the cause of complete immobility of the limb and disability.
Stage 1 symptoms:
- Aching, dull pain that disappears after rest.
- Occasionally discomfort in the groin and knee.
Stage 2 symptoms:
- pain with slight exertion, at night, after rest ("starting");
- characteristic crunch or crackle during movement;
- it is difficult to bend and abduct the limb;
- gait changes are formed, a person is limping, waddles from foot to foot;
- muscles spasm (involuntarily contract), over time, greatly decrease, lose strength.
Stage 3 symptoms:
- pain is felt constantly;
- pronounced crunch or crackle;
- muscles are atrophied;
- the leg is shortened (lengthened in 10% of cases) - due to the destruction of the cartilage and a decrease in its height;
- movement in the joint is almost impossible;
- a person is practically unable to move without assistance.
With the further development of the pathological process, complete disability occurs.

Possible complications
- Dying off of tissues.
- Protrusion (pushing) of the acetabulum.
- Spinal deformity (kyphosis and scoliosis).
- Knee arthrosis (gonarthrosis).
- Arthritis, bursitis (acute inflammation of the tissues of the joint).
- Ankylosis (tissue fusion, complete immobility of the leg).
Diagnostics
The main method for diagnosing hip arthrosis is radiography. With its help, the degree of the disease is determined.
Sometimes, to determine the state of soft tissues, it is necessary to additionally undergo CT or MRI.
Indicators of laboratory tests (general and biochemical blood test, coagulogram - blood clotting test, urinalysis) with arthrosis remain unchanged.
However, with concomitant inflammation of the synovial capsule (reactive synovitis):
- the erythrocyte sedimentation rate (ESR) increases;
- the level of sialic acids and seromucoids (substances that indirectly indicate the presence of inflammation) increases.

Treatment methods
Based on the results of the diagnosis, the doctor determines the degree of joint damage and how to treat it. The disease cannot be completely cured. In the first two stages, it is possible to stop it with drugs. Later, mobility can be restored only through endoprosthetics.
Conservative treatment
The doctor prescribes a set of medications that eliminate pain, tissue inflammation, muscle spasm, and improve the condition of the cartilage.
How to treat a patient in an exacerbation stage:
| Drug group name | Effect |
|---|---|
Chondroprotectors |
Restrain and prevent the destruction of cartilage, improve the composition of the synovial fluid and nutrition of chondrocytes |
Anti-inflammatory non-hormonal drugs |
Eliminate pain and inflammation |
Muscle relaxants |
Relieve spasm |
Hormonal agents |
They have analgesic, anti-allergic, anti-edematous and strong anti-inflammatory effects |
Vasodilators |
Eliminate spasm, improve blood circulation and enhance the supply of nutrients to the periarticular tissues, promote their rapid recovery |
Ointments, liquids, topical cream |
Improve microcirculation and metabolism in tissues, irritate, relieve pain, relieve inflammation |
Physiotherapy
To speed up metabolism and tissue repair, the disease is treated with physiotherapy methods:
- mud applications;
- overheating with paraffin or ozokerite ("odorous wax"; natural fossil of the petroleum group);
- electrical stimulation (exposure to impulse currents of various frequencies);
- laser therapy (treatment using optical radiation);
- ultrasound therapy (the procedure heals with high-frequency mechanical vibrations);
- acupuncture (acupuncture);
- therapeutic massage.
The mobility of the thigh is also restored by a special procedure - traction (hardware traction). Stretching the joint capsule, they give the correct position to the articular surfaces, relieve them of the load. The disease is treated with a course of 10-12 procedures.

Exercises exercise therapy
To strengthen the muscles and ligaments of the thigh with 1 and 2 degrees of the disease, exercise therapy is prescribed.
During the recovery period, exercises are performed under the guidance and supervision of a physiotherapist (in a hospital).
Physiotherapy:
- Lying on your stomach, slowly raise your leg 15–20 cm, lock and hold as long as you can (up to 30 seconds).
- Lying on your side, slowly pull your bent knees to your chest (as far as possible).
- From the same position, bend the leg under you at the knee, straighten the other and raise it above the floor by 45 degrees, holding for 20-30 seconds.
- Lying on your back, put your hands under your head, spread your legs bent at the knees shoulder-width apart. Slowly raise the pelvis, hold this position for 10-15 seconds, lower it (the effect of the exercises will be ifarthrosis of the hip joint to treatin this way daily).
- Repeat the previous exercise with your knees together.
- Stand with your feet apart (shoulder-width apart), bend over and touch your foot without bending your knees.
- Lying on your back, raise your legs straight and pull your socks towards your head, trying to touch the floor (behind your head)
- In the same position, bend your knees, connect them together, turn left and right, trying to touch the floor with your knees. Press your back and shoulders to the floor.
- Sit down with your knees shoulder-width apart, bring your knees together and apart (gradually wider).
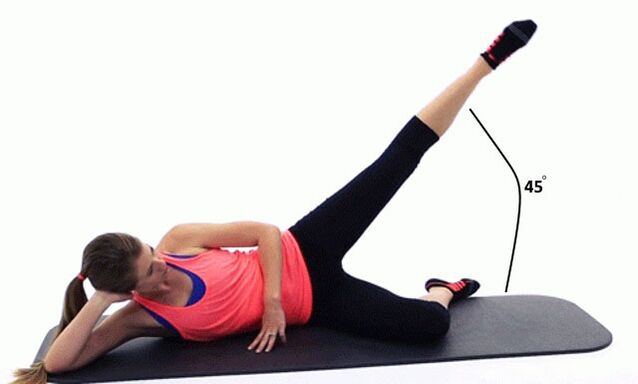


Repeat each exercise 10-15 times daily, do them slowly and without tension.If you experience any unpleasant or painful sensations, cancel classes.
When an operation is needed
Surgical intervention is necessary:
- if the pathology progresses;
- when the patient is worried about severe, persistent pain;
- if the deformation of the joint interferes with full movement;
- at stage 3 of the disease.
Arthroplasty
Arthroplasty is a type of surgical correction.
It is produced in the early stages of the disease with:
- deformities of the joints;
- destruction of cartilage;
- the appearance of contracture (tissue fusion, fixation of the thigh in a forced position).
With arthroplasty, the articular surfaces are corrected:
- Fragments, cartilaginous growths, foci of necrosis are removed.
- They give the articular surfaces a normal anatomical shape (reduce, remove bone growths) and grind.
- Depressions and irregularities are filled with plastic material (artificial implant).
Then the anatomical parts of the joint are aligned and reinforced with metal plates.
After arthroplasty:
- on days 4–5, the patient is allowed to sit down;
- after 1. 5–2 weeks - walk, leaning on crutches;
- after 3 weeks - work out the hip with exercise therapy and walk without crutches.
In the same period, physiotherapy procedures (therapeutic massage) are prescribed.
Full recovery takes 2 to 6 months.
Endoprosthetics
Surgical treatment of arthrosis of the hip joint or replacement with an artificial implant is prescribed in the later stages, as well as for joint deformities that cannot be corrected by other methods.
Endoprosthetics technique:
- remove the cartilage of the acetabulum and the head of the hip bone, grind the surface;
- an artificial glenoid cavity is implanted, and instead of the head of the joint - a hinge on the leg;
- the implants are fixed with medical cement or by drilling a channel into which the prosthesis is screwed;
- combine parts of the joint;
- check his work (bending-unbending the leg);
- reinforced with metal plates.
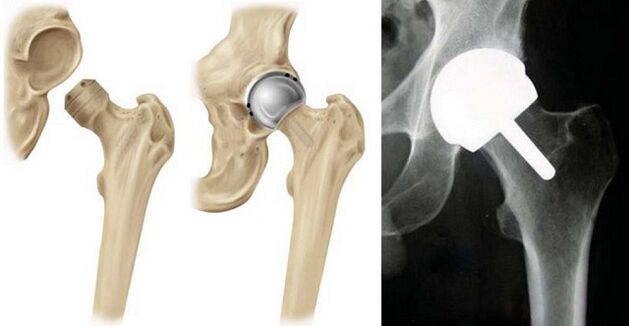
The recovery period is the same as after arthroplasty.
The prosthesis functions up to 20 years. In 97% of cases, leg functions are fully restored (even sports loads are allowed).
Prevention
For the prevention of arthrosis, it is necessary to take general measures to promote health:
- Adjust your diet with the help of your doctor.
- Lead an active lifestyle.
- Protect the joint from excessive stress.
- Don't overcool.
- Avoid uncomfortable shoes.
To prevent further destruction of the joint with existing arthrosis, it is recommended:
- constantly engage in physiotherapy exercises;
- to carry out sanatorium-resort treatment annually;
- repeat the course of therapeutic massage 2-3 times a year.
Disease prognosis
Coxarthrosis is one of the most common and severe forms of deforming arthrosis (60% of all arthrosis cases). The disease cannot be completely cured. It progresses throughout life.
In the early stages (1 and 2), conservative methods (exercise therapy, massage, medications) can pause the development of pathology, delay the onset of severe symptoms for 5 years (and more).
At a late stage (3), the disease leads to immobilization of the diseased joint (this is a disability of groups 1, 2 or 3). In this case, arthroplasty is performed, after which functions are restored in 97% of cases.
















































